Starting with Why: DST for Patient Engagement and Quality Improvement
Written by Mike Lang, CLDST Level 3 Facilitator
Screen Capture from the Patient Stories Platform on the Alberta Health Services website.
Introduction: Why Start with Why
In his famous 2010 TED Talk entitled "Start with Why," Simon Sinek states that many organizations know what they do and how they do it, but "very few organizations know why they do what they do." He emphasizes that a lack of clarity around this question is one of the biggest challenges in large organizations, separating the successful from the unsuccessful. Healthcare systems are not immune to this challenge as both the practice and planning of healthcare can become process-oriented, unintentionally forgetting the reason for its existence in the first place: promoting and protecting the health of a population. Healthcare providers, administrators, and professionals have long recognized that centering the patient and their family in all aspects of operations and service planning is essential to providing high-quality care. Patient and family stories can help remind healthcare providers why continuous quality improvement is important as well as cultivate patient-and-family-centered care by influencing the psychological factors of "readiness for change" (i.e., beliefs, attitudes, and values).
This case study chronicles the experience of a large healthcare organization, Alberta Health Services (AHS), in developing a program to develop and share compelling patient and family-created Digital Stories to assist in quality improvement initiatives. For context, AHS is Canada's first and largest province-wide, fully integrated health system. AHS is responsible for delivering health services to 4.4 million residents and comprises more than 103,000 direct employees, 15,100 volunteers and 10,800 physicians. In the words of former AHS CEO, Dr. Verna Yiu, the Digital Storytelling program is designed to help remind AHS employees and volunteers of "why we are here in the first place" and contribute to a shift in mindset away from "what is the matter with you" and towards "what matters to you."
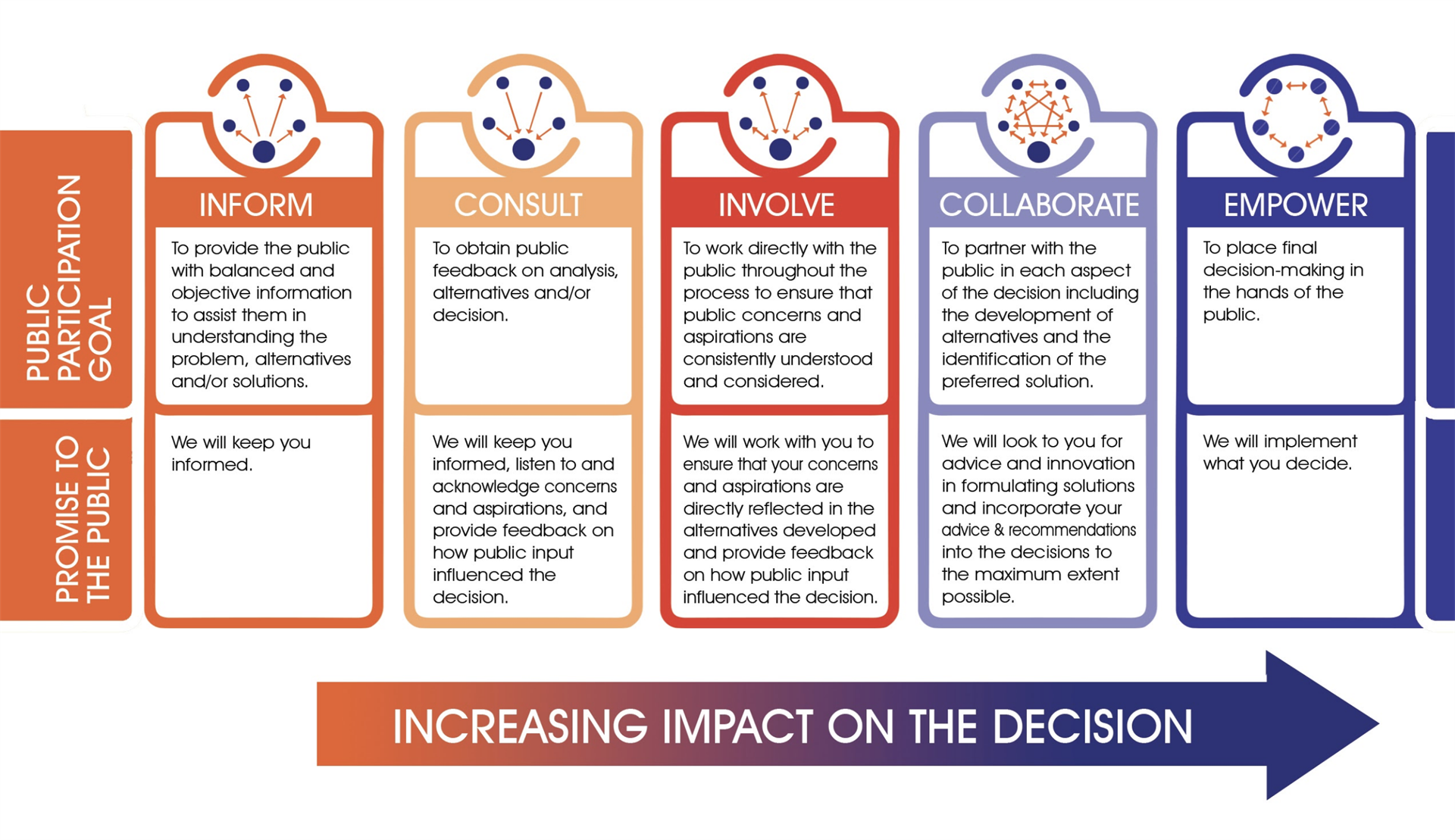
IA2P Spectrum of
Public
Engagement
iap2canada.ca/foundations
In Demand: Patient Engagement in a Large Healthcare Organization
AHS recognized the ability of patient and family advisors (from now on referred to as advisors) to contribute to the improvement of healthcare systems and contextualize important healthcare conversations and this led to the formation of the department of Experience and Patient Engagement (EPE) in 2009. One of EPE’s initial goals was to foster an active and growing network of advisors to partner with quality improvement initiatives across the organization. Over time, the advisors were increasingly asked to share their stories in meetings, conferences, and planning sessions. Given the increasing frequency of requests, the EPE team became interested in building the capacity of advisors to effectively communicate and share their personal stories while also looking for ways to minimize the burden associated with attending numerous meetings and continuously retelling their story. Initially, written stories were produced using one-on-one interviews and these were provided to the requesting group. However, this approach was time-consuming, and the written stories were unsuccessful in conveying the full emotional impact of patient and family experience. It was also recognized that most of these engagement requests fell within the "inform," "consult," or "involve" categories on the IAP2 Spectrum of Public Participation.
There was a need for more meaningful engagement initiatives on the "collaborate" and "empower" side of the continuum.By 2015, the EPE team was managing more than 800 advisors and began to explore new ways to meet the growing demand for inclusion of the patient and family voice in planning and practice. At this time, Digital Storytelling (DST) was highlighted as a “collaborate/empower” engagement opportunity that could improve storytelling skills and also produce profoundly impactful stories to meet the increased demand. The EPE team recognized that the short duration and compelling nature of a digital story could make them easier to embed into routine clinical practice and enhance patient-Centred care. The stories could also be tied to specific quality improvement and educational initiatives related to patient experience on a broad scale while at the same time reducing the onerous amount of storytelling requests placed on advisors. As DST facilitation in a healthcare context requires a unique skillset and significant experience, the decision was made to hire an outside DST professional. Mike Lang (Level 3 facilitator with Common Language) was hired to help develop digital stories with advisors and build DST facilitation capacity within the EPE team.
Mike Lang facilitating one of the first DST Workshops with AHS.
Circa. 2015.
Finding, Crafting, Safeguarding: A Brief Overview of the Digital Storytelling Process in AHS
The implementation of the DST initiative began with extensive planning and discussion to ensure that it was done effectively and ethically. However, as with all new initiatives of this scale, there was constant experimentation and adjustments made. Some of the considerations and procedures that were essential to the DST project's success are described below.
Logistical Considerations
A traditional DST workshop format involves 6-10 participants working in the same location over three consecutive days. They each write their own story, record their voiceover, and edit their story together. However, in the AHS context, it was quickly determined that this format would not be feasible for advisors due to their health situations and caregiving responsibilities. Therefore, a two-pronged approach was created with some advisors with limited availability working one-on-one with the DST consultant for three, two-hour sessions to create their digital story (Individual; the focused facilitation of the one-to-one approach reduced the time commitment). In contrast, others participated in a modified workshop format (Group). The group workshop included a three-hour introductory webinar to begin the story writing process and two eight-hour, in-person days over a single weekend. To efficiently utilize available staff resources and support the creation of 15-20 digital stories per calendar year, 6-8 advisors were invited to two separate group workshops with three advisors creating stories one-on-one with the consultant.
To achieve appropriate provincial representation, each of the five health Zones hosted one workshop with patient advisors recruited from that Zone. Given the vast geography of the province, bringing the workshops to the local area reduced travel for the participants and allowed them to tend to family/caregiving responsibilities. The DST consultant facilitated all the workshops with the EPE DST lead and Zone EPE representative acting as co-facilitators. All workshop equipment was provided by the DST consultant with all other logistics coordinated by the EPE department.
Ethical Considerations
Although a commitment to storyteller wellbeing requires an individually contextualized, or "situated," ethical practice, there were specific concepts (eg., continual consent) and procedures (eg., clear project goals/expectations, awareness of story implications, ownership, etc.) that guided our ethical decision making for the creation and screening of digital story within AHS. One example of an ethical consideration in this project was around ownership. As a healthcare organization, it was not ethical to assert ownership over patient- and family-created stories. Therefore, it was made clear from the beginning that each advisor owns their digital story and allowing AHS to share the story on their behalf to maximize its impact. This could be viewed as an organizational risk (i.e., investing resources into a process that does not result in ownership). However, in our experience, when participants clearly understand the goals and expectations of the project, are involved in a continual consenting process, and recognize that their wellbeing is the primary concern, they are excited to have their story shared widely. Through the rigorous, situated ethical practice of DST, both storyteller wellbeing and organizational goals can be achieved.
Participant Experiences
The response of DST workshop participants was overwhelmingly positive, with 100% of participants who filled a post-workshop evaluation in the first one and a half years of the project (n=22) strongly agreeing that "Overall, I felt the workshop was rewarding and a good use of my time." Other feedback included strong endorsement of the statements: a) "I am excited to share my story with others" (n=22, strongly agree = 17, agree = 3, slightly agree = 2), b) "I believe the information I learned in this workshop will be useful in my role as a patient or family advisor" (n=16, strongly agree = 13, agree =1, slightly agree = 2), and c) “As a result of attending this event, I feel more connected with the goal of AHS to improve patient and family experience" (n=16, strongly agree = 14, agree = 1, slightly agree = 1). Across all Likert-type evaluation questions, there were no negative responses.
Qualitative feedback included statements such as:
a) "It was an incredible weekend full of profound moments. Sitting with the other participants and hearing their story's [sic] was the highlight for me."
b) "It provided me with an opportunity to dig deeply into my past journey (positive and negative), look at the pains and joys I have experienced,
and accept them as part of who I am today."
c) "I am so excited to know that this is a priority for AHS, and that the experiences of patients and families are considered and valued."
d) "Most powerful workshop I have attended."
Finally, as the DST workshop was part of an ongoing relationship with the patient and family advisors who participated, follow up communications in the months and years following the workshop included statements like,
a) "Before making my digital story, when I would talk about what happened, it made me feel fragile and since making the story, talking about it
now somehow the pain of it is gone. It made me stronger."
b) "I use mine all the time at every speaking event I do. I don't have to keep rehashing the trauma but instead can concentrate on what I want to
be different as a result of what happened to me."
Overall, the DST process used was found to be both useful and meaningful for advisors. However, this only represents a small part of the impact of the program. In the final section, we will examine the use and impact of the DS that have been created.
Mike Lang with a group of patient advisors at a Digital Storytelling workshop in Grand Prairie, AB.
Circa. 2019
Focused, Powerful, Engaging: Use of Patient- and Family-Created Digital Stories
The EPE department now curates a public playlist of over 100 patient- and family-created DS encompassing numerous disease groups, disciplines, and geographic areas of the province. The stories have a combined view count of over 200,000 views (as of September 2022) and are shared on the front facing AHS website (ahs.ca/patientstories). Early in the development of the DST AHS program, the EPE team began utilizing digital stories to anchor presentations, workshops, coalition meetings, internal and external campaigns, documents, research projects, and healthcare conferences with the patient and family voice. Quickly, digital stories became a critical tool that the EPE team employed to stimulate conversations about person-centered care with leaders, physicians, and teams. It was observed that digital stories were able to move the primary focus of the conversation away from system barriers and logistical challenges (problem-based approach) towards providing the best care to patients and families (solutions-based approach). This shift in focus increased collaboration and engagement by aligning quality improvement initiatives with healthcare providers' core ethical principles (i.e., providing the best possible care). It was also observed that digital stories cultivated empathy for patients and families by providing additional context for healthcare interactions and exploring their inner emotional experience of illness or injury. Together, the shift in focus of conversations and empathetic response cultivated a readiness for change and today, the EPE team fields requests from leaders across AHS to strategically identify stories for specific meetings, presentations, or initiatives. EPE staff frequently recommend stories to groups seeking a way to better understand and reflect on the patient experience. Many advisors who created a digital story also share it regularly in their advisory roles and with family and friends and other advocacy activities with non-profit organizations and online communities.
The value of DST is now recognized throughout AHS and has led to additional practice areas sponsoring digital story production. New DST projects outside the core EPE DST program have been initiated by primary health care, seniors care, palliative and emergency strategic clinical networks, as well as through specific grant-funded projects with indigenous health, cancer care, pediatrics, social work, and public health. The Patient and Family Stories playlist has received sponsorship from AHS leadership who routinely include digital stories in their presentations to bring the patient and family voice to various audiences across the organization. Currently, continuing to leverage the interest in DST and build momentum for the DST program is the EPE team's central focus.
It has been widely recognized by AHS and other large healthcare organizations that stories are the basis for how culture is formed and perpetuated. Storytelling can be used to cultivate engagement, reflection, and collaboration between healthcare providers and patients and families. The challenge for large healthcare systems is to share stories in the most compelling and accessible way possible to realize these benefits. The DST program in AHS has not only provided patient and family advisors with meaningful, and often therapeutic, engagement opportunities, it has stimulated meaningful discussions within the healthcare system. From our experience, a good story, well told in digital story form can help nudge large organizations towards more patient- and family-centered care generally, as well influence the success of specific quality improvement initiatives, by starting with why.
Mike Lang facilitating a digital story screening with a group of healthcare providers in AHS.
Circa. 2020